Blog & News

Addressing Persistent Medicaid Enrollment and Renewal Challenges as Rolls Increase
September 2, 2020:
Growth in Medicaid enrollment is expected to accelerate as a result of both the COVID-19 pandemic and the associated economic downturn. An analysis by the Kaiser Family Foundation (KFF), for example, shows that by January 2021, nearly 17 million people could be newly eligible for Medicaid. i In June, the Georgetown Center for Children and Families reported that Medicaid enrollment in 15 states had increased 5.8 percent over the past three months. ii The additional expected increase could mirror the surge seen during the first Patient Protection and Affordable Care Act (ACA) Open Enrollment Period (OEP1) in 2013, during which there was an influx of first-time applicants who were unfamiliar with Medicaid enrollment and renewal processes.
Although significant progress has been made in streamlining and simplifying these processes and systems for beneficiaries whose income eligibility is determined based on modified adjusted gross income (MAGI), states vary widely in their priorities and approaches. iii There are still many points along the enrollment and renewal paths where eligible individuals might remain uninsured or lose Medicaid coverage, and these challenges may be exacerbated by a surge in newly eligible individuals. Recently, some states have taken advantage of the flexibility in enrollment and eligibility determination offered by the COVID-19 Public Health Emergency (PHE) declared by Health and Human Services Secretary Alex Azar in order to streamline Medicaid enrollment processing iv v vi vii viii ix ; however, this flexibility may be rolled back at the end of the PHE while widespread enrollment and renewal challenges will continue to persist.
Drawing on work done for the Medicaid and CHIP Payment and Access Commission (MACPAC), this blog provides a summary of documented, effective mitigation strategies states can use to address enrollment and renewal challenges in Medicaid and highlights strategies currently being used in four states: California, Idaho, Rhode Island, and Washington. Although this analysis pre-dates the coronavirus outbreak, these findings may offer helpful ideas about how states can address long-standing challenges in enrolling and renewing individuals in Medicaid as during current nationwide enrollment increases nationwide due to COVID-19 as well as in anticipation of returning to regular operations once the PHE expires. The findings, statements, and views expressed here are those of the authors and do not necessarily represent those of MACPAC.
Overview: Challenges and Mitigation Strategies
Trends in state Medicaid and CHIP eligibility, enrollment, and renewal policies over the past four years indicate that an increasing number of states are complying with ACA provisions designed to streamline program administration at enrollment and renewal. x States are also moving toward providing more application supports, which can make the process faster and more user-friendly, as shown in Table 1.
| Table 1. Application Supports Aimed at Streamlining Enrollment |
| Indicator from Kaiser/Georgetown Survey | # of States as of |
| January 2017 | January 2018 | January 2019 | January 2020 |
| Online application submission using mobile device | 28 | 31 | 38 | 44 |
| Online application has mobile-friendly design | 7 | 9 | 18 | 20 |
| Online beneficiary account supports uploading of verification documentation | 29 | 31 | 32 | 33 |
| Online secure portal for application assister | 26 | 27 | 27 | 30 |
Note: The survey denominator is 50 states and D.C. Forty-one states supported online beneficiary accounts in 2017, 42 states supported them in 2018 and 2019, and 43 states supported them in 2020.
Sources: Brooks, T., Wagnerman, K., Artiga, S., Cornachione, E., and Ubri, P. 2017. Medicaid and CHIP eligibility, enrollment, and cost sharing policies as of January 2017: Findings from a 50-state survey. Washington, DC: Georgetown CCF and KFF. Available at http://files.kff.org/attachment/Report-Medicaid-and-CHIP-Eligibility-as-of-Jan-2017; Brooks, T., Wagnerman K., Artiga S., and Cornachione, E. 2018. Medicaid and CHIP eligibility, enrollment, and cost sharing policies as of January 2018: Findings from a 50-state survey. Washington, DC: Georgetown CFF and KFF. Available at http://files.kff.org/attachment/Report-Medicaid-and-CHIP-Eligibility-Enrollment-Renewal-and-Cost-Sharing-Policies-as-of-January-2018; Brooks, T., Roygardner, L., and Artiga, S. 2019. Medicaid and CHIP eligibility, enrollment, and cost sharing policies as of January 2019: Findings from a 50-state survey. Washington, DC: Georgetown CFF and KFF. Available at http://files.kff.org/attachment/Report-Medicaid-and-CHIP-Eligibility-Enrollment-Renewal-and-Cost-Sharing-Policies-as-of-January-2019; Brooks, T., Roygardner, L., Artiga, S., Pham, O., and Dolan, R. 2020. Medicaid and CHIP eligibility, enrollment, and cost sharing policies as of January 2020: Findings from a 50-state survey. Washington, DC: Georgetown CFF and KFF. Available at http://files.kff.org/attachment/Report-Medicaid-and-CHIP-Eligibility,-Enrollment-and-Cost-Sharing-Policies-as-of-January-2020.pdf |
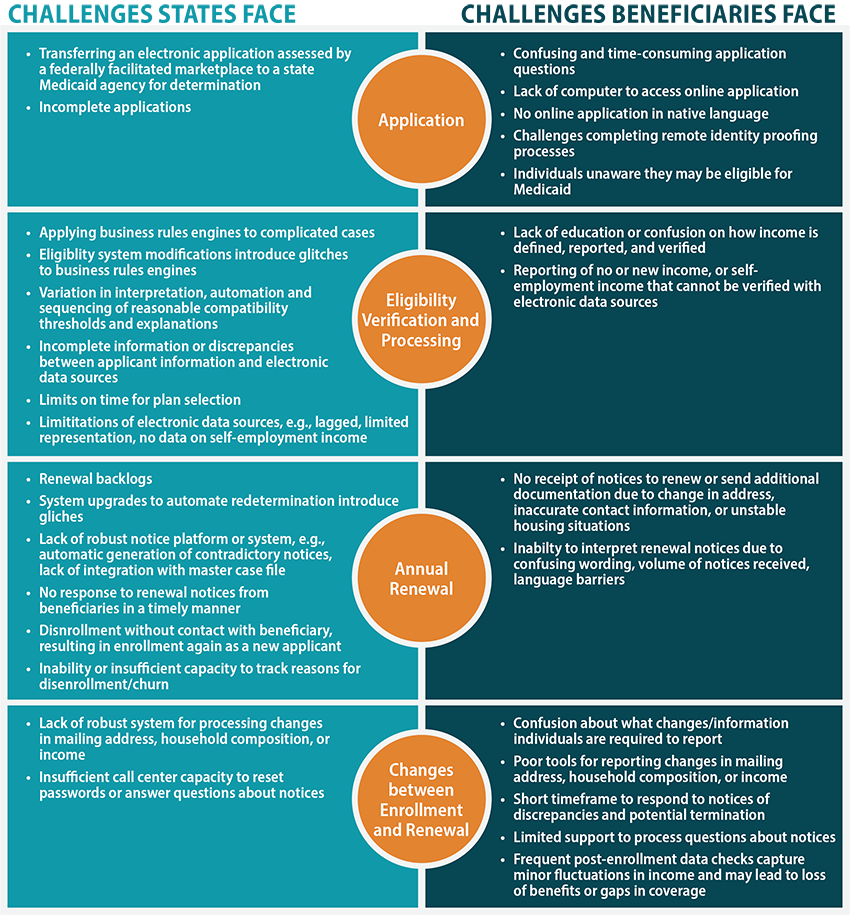
Through document review and key informant interviews, we identified 30 ongoing Medicaid enrollment and renewal challenges, many of which are longstanding issues that predate state streamlining efforts and the COVID-19 outbreak. Exhibit 1 shows the different challenges states and beneficiaries may face at each point of the Medicaid application, income verification, and renewal processes, as well as the points between enrollment and renewal.
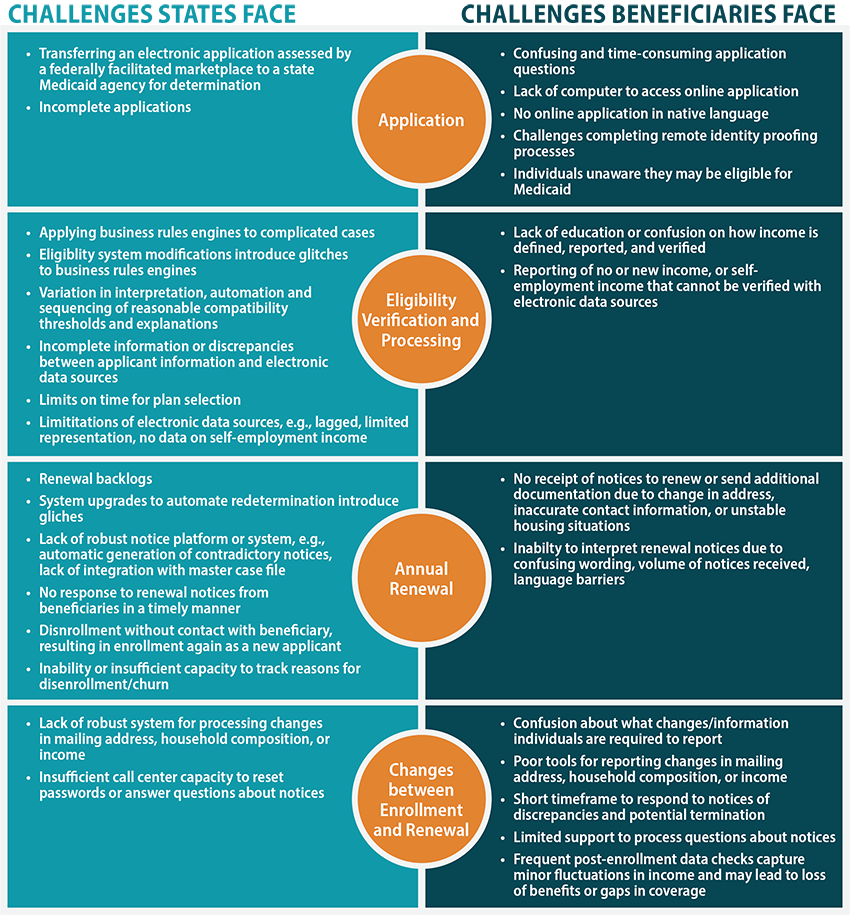
Exhibit 1. Remaining MAGI Medicaid Enrollment and Renewal Challenges
Source: State Health Access Data Assistance Center (SHADAC) document review and select key informant discussions 2020.
We also reviewed the robust body of literature on effective strategies for increasing MAGI Medicaid enrollment, and we compiled and organized some of the most effective strategies that states can implement at each point of the Medicaid enrollment and renewal processes (Exhibit 2).
- Offer application assistance through assister portals, in-person application assistance, or application assister call centers (MAC Learning Collaborative 2019)
- Help applicants find and connect with local assisters (Wishner 2018)
- Create consumer-friendly application tools and prompts that allow applicants to provide the most complete and accurate information possible (Brooks, Park, and Roygardner 2019; CBPP 2020; MAC Learning Collaborative 2019; Wishner 2018)
- Use a dynamic application that responds to an applicant’s unique characteristics (MAC Learning Collaborative 2019)
- Shorten applications or expedite the application process (Code for America 2019)
- Combine a state’s Medicaid application with applications for other social safety net programs (Code for America 2019)
- Create an express lane or presumptive eligibility option for certain applicants (Brooks, Park, and Roygardner 2019)
- Couple strategies with different modes and intervals of outreach (Maneely 2019)
- Enable applicants to upload necessary documents into their application (MAC Learning Collaborative 2019)
- Follow up by telephone for incomplete applications (MAC Learning Collaborative 2019)
- Allow self-attestation of income, including attestation of no income or self-employment, without further documentation requirements (Wagner 2016; Wishner 2018)
- Leverage linkages to all available electronic data sources—including but not limited to state and federal data sources as well as data from other safety net programs such as SNAP, TANF, etc.—to verify applicant eligibility (Brooks, Roygardner, and Artiga 2019; MACPAC 2019; Wagner 2018)
- Reference the National Change of Address (NCOA) database and other eligibility verification sources regularly to keep case information current (Lynch 2019; Wagner 2018)
- Integrate information validation procedures and verification data sources into the application process (MAC Learning Collaborative 2019)
- Send alerts if reported income differs from data sources by reasonable compatibility standard, automate flags for individuals reaching milestones like aging or pregnancy to avoid incorrect eligibility category assignments (GAO 2020)
- Involve eligibility workers in complicated eligibility determinations and create a specialized task force in each state to handle complicated eligibility determinations (MAC Learning Collaborative 2019)
- Cease sending notices if application discrepancies do not affect eligibility determination (Wagner 2016)
- Automatically renew Medicaid benefits (Artiga and Diaz 2019)
- Send more than one follow-up request for non-response to renewal notices (Brooks, Park, and Roygardner 2019)
- Improve the clarity and content of renewal notices (Brooks, Park, and Roygardner 2019)
- Consider switching to an annualized income policy or 12-month continuous eligibility (Brooks, Park, and Roygardner 2019; Wishner 2018)
- Engage with managed care organizations both to assist with renewal of benefits (Brooks, Park, and Roygardner 2019)
During our analysis we identified two persistent risk points that are especially relevant during the COVID-19 pandemic: verifying self-employment income and making eligibility determinations for complicated cases. Below we highlight effective mitigation strategies that California, Idaho, Rhode Island, and Washington have implemented to address these challenges.
Challenge: Verifying Self-Employment Income.
Income verification remains one of the biggest challenges states face when determining an individual’s financial eligibility for Medicaid. xi This is especially true for those with unstable incomes, such as individuals who are self-employed, seasonally employed, or frequently change jobs. In these cases, income may not be able to be confirmed with electronic income data sources due to data lags or other limitations. When electronic sources cannot be used, alternative documentation is required (e.g., pay stubs). Further, individuals reporting self-employment income often have to submit additional financial information, compared to those who are not self-employed, in order to verify their income. This information may include recent tax filings or profit and loss statements (i.e., summaries of revenues, costs, and expenses that were incurred during a specific period). Collecting and reporting this information can be confusing and difficult, especially for new Medicaid enrollees.
Mitigation Strategy: Offer multiple options for reporting and verifying self-employment income.
- Allow multiple forms of documentation (e.g., bank statements or self-created profit and loss statements, or self-attestation) to report self-employment income. California and Idaho both allow self-employed individuals to verify income by submitting their own self-generated profit and loss statement or a summary of their expected income generated by a certified public accountant. Both states have also created alternative forms that mirror the income and expense categories typical for self-employed individuals and can be used to help self-employed applicants or beneficiaries report their net income.
- Provide flexible tools that help self-employed individuals accurately calculate their income. Washington’s online Medicaid application includes a built-in income calculator, which assists individuals with accurately reporting their income in a variety of increments (e.g., hourly, monthly, quarterly, or annually) and then prompts individuals with additional questions in order to determine financial eligibility.
Mitigation Strategy: Clearly explain what individuals need to report and how to report it.
- Provide explicit direction about what counts as income for MAGI purposes. California has worked collaboratively with community stakeholders to create a “What Income Counts” document xii that explains what income to report and how to report it. Similarly, Washington has a dedicated webpagexiii with guidance for self-employed individuals to calculate income and provides helpful examples of business expenses to deduct from this calculation.
- Provide education and referrals to help applicants collect needed documentation. Respondents indicated that in-person assistance from navigators and enrollment assistors remains a critical tool for individuals to successfully report their income upon initial application and at times of renewal. For example, in Idaho, navigators report success in scheduling pre-appointments with applicants to review what documents are needed for the application. Similarly, navigators in Washington indicate that tax accountants (e.g., United Way free tax preparers) have become an important referral for individuals who need help calculating profit and loss statements.
Challenge: Making Swift and Accurate Eligibility Determinations for Complex Cases.
Robust business rules engines (software systems that automate Medicaid rules as well as electronic access to data sources to verify various factors of eligibility) have been critical tools to support successful and real-time Medicaid eligibility determinations. This is especially true for simple cases, such as a single adult with relatively stable employment. Some states, however, continue to struggle with business rules engines making correct determinations in more complex enrollment situations, such as families with mixed health insurance coverage or individuals missing information on key eligibility factors.
Mitigation Strategy: Deploy a specifically trained workforce and formalize escalation procedures to resolve issues in the eligibility system.
- Create a category of navigators authorized to move more complex cases through the application or renewal process. Washington provides additional training to “enhanced” navigators who offer technical assistance to regular navigators in order to troubleshoot problems that arise when processing complex cases. Enhanced navigators attend additional training throughout the year to receive updates on processes and policies, and they have a higher level of access to the eligibility system.
- Provide a mechanism to escalate cases. Rhode Island provides navigators with the ability to escalate cases that appear to have received incorrect eligibility determinations, especially in situations where there is a quick-turnaround time needed—e.g., medical emergencies. Escalation teams within the state’s human services agency are designated to respond to navigators in a timely manner with a determination review.
Mitigation Strategy: Utilize community feedback mechanisms to identify enrollment challenges with complex cases and identify mitigation solutions.
- Interviewees in all four states (California, Idaho, Washington, and Rhode Island) highlighted the importance of community feedback mechanisms in providing a venue for navigators to bring developing challenges and areas of concern to the attention of the state and to suggest solutions. Specifically, stakeholders in California and Washington spoke positively about the increasing number of opportunities—such as formal consumer-focused stakeholder workgroup meetings or informal communication channels—for navigators, eligibility workers, and community organizations to collaborate regularly with state agency staff to discuss complex cases and consider ways to better address these situations.
Conclusion
Our analysis focused on identifying effective and innovative strategies for addressing Medicaid enrollment and renewal challenges and exploring specific strategies used by four states—California, Idaho, Washington, and Rhode Island. Since this study, the spread of the COVID-19 virus has simultaneously increased the need for medical coverage to cover fees associated with COVID treatment and triggered an economic downturn, and both of these issues are expected to increase enrollment in Medicaid programs nationwide. xiv While the administrative flexibilities mentioned earlier aim to facilitate the influx of new Medicaid enrollments for the time being, the main risk points of Medicaid enrollment and renewal can be expected to continue in some form and will no doubt return when the Public Health Emergency ends. xv The need to continue to explore and implement innovative enrollment and renewal approaches remains, and the findings from this analysis can offer a reminder to states of ongoing efforts to improve Medicaid enrollment and renewal processes.
References:
i Eligibility for ACA Health Coverage Following Job Loss. Washington, DC: Kaiser Family Foundation (KFF). Available at https://www.kff.org/coronavirus-covid-19/issue-brief/eligibility-for-aca-health-coverage-following-job-loss/
ii Alker J. (June 18, 2020). Medicaid Enrollment Appears to be Accelerating. Washington, DC: Georgetown Center for Children and Families. Available at https://ccf.georgetown.edu/2020/06/18/medicaid-enrollment-appears-to-be-accelerating/
iii Zylla E., Planalp C., Lukanen E., and Blewett L. (February 2018). Section 1115 Medicaid Expansion Waivers: Implementation Experience. Contractor Report for the Medicaid and CHIP Payment and Access Commission (MACPAC). Minneapolis, MN: State Health Access Data Assistance Center (SHADAC). Available at https://www.macpac.gov/wp-content/uploads/2018/02/Section-1115-Medicaid-Expansion-Waivers-Implementation-Experiences.pdf
iv Schubel, J. (June 18, 2020). States Are Leveraging Medicaid to Respond to COVID-19. Washington, DC: Center on Budget and Policy Priorities (CBPP). Available at https://www.cbpp.org/research/health/states-are-leveraging-medicaid-to-respond-to-covid-19
v Wagner J. (May 13, 2020). Streamlining Medicaid Enrollment During COVID-19 Public Health Emergency. Washington, DC: Center on Budget and Policy Priorities (CBPP). Available at https://www.cbpp.org/research/health/streamlining-medicaid-enrollment-during-covid-19-public-health-emergency
vi Boozang, P., and Serafi, K. (April 29, 2020). State Strategies to Support Medicaid/CHIP Eligibility and Enrollment in Response to COVID-19. Princeton, NJ: State Health and Value Strategies (SHVS). Available at https://www.shvs.org/wp-content/uploads/2020/04/State-Strategies-to-Support-Medicaid_CHIP-Eligibility-and-Enrollment-in-Response-to-COVID-19.pdf
vii Medicaid and CHIP MAC Learning Collaborative. (August 20, 2018). Disaster Preparedness Toolkit for State Medicaid Agencies. Washington, DC: Centers for Medicare and Medicaid Services (CMS). Available at https://www.medicaid.gov/state-resource-center/downloads/mac-learning-collaboratives/medicaid-chip-disastertoolkit.pdf
viii Hill, I., Haley, J.M., and Burroughs, E. (March 19, 2020). Medicaid and CHIP Flexibility Can Help Safeguard Americans during the COVID-19 Crisis. Washington, DC: Urban Institute. Available at https://www.urban.org/urban-wire/medicaid-and-chip-flexibility-can-help-safeguard-americans-during-covid-19-crisis
ix Artiga, S., Rudowitz, R., and Musumeci, M. (March 17, 2020). How Can Medicaid Enhance State Capacity to Respond to COVID 19? Washington, DC: Kaiser Family Foundation (KFF). Available at https://www.kff.org/coronavirus-covid-19/issue-brief/how-can-medicaid-enhance-state-capacity-to-respond-to-covid-19/
x Zylla, E., Au-Yeung, C., Lukanen, E., and Worrall, C. (October 19, 2018). Assessment and Synthesis of Selected Medicaid Eligibility, Enrollment, and Renewal Processes and Systems in Six States. Contractor Report for the Medicaid and CHIP Payment and Access Commission (MACPAC). Minneapolis, MN: SHADAC. Available at https://www.macpac.gov/publication/assessment-and-synthesis-of-selected-medicaid-eligibility-enrollment-and-renewal-processes-and-systems-in-six-states/
xi Zylla E., Planalp C., Lukanen E., and Blewett L. (February 2018). Section 1115 Medicaid Expansion Waivers: Implementation Experience. Contractor Report for the Medicaid and CHIP Payment and Access Commission (MACPAC). Minneapolis, MN: State Health Access Data Assistance Center (SHADAC). Available at https://www.macpac.gov/wp-content/uploads/2018/02/Section-1115-Medicaid-Expansion-Waivers-Implementation-Experiences.pdf
xii California Department of Healthcare Services. (nd). MAGI-Based Medi-Cal: Whose Income Counts in the Household Calculation? Sacramento, CA: California Department of Healthcare Services. Available at https://www.dhcs.ca.gov/services/medi-cal/eligibility/Documents/Co-OPS-Sup/Whose_Income_Counts_Flowchart.pdf
xiii Washington State Department of Social and Health Services, Economic Services Administration. (November 6, 2019). Olympia, WA: Washington State Department of Social and Health Services. Automated Client Eligibility System (ACES): Modified Adjusted Gross Income (MAGI) Medical. Available at https://www.dshs.wa.gov/node/1981/
xiv Rudowitz R., and Hinton E. (May 15, 2020). Early Look at Medicaid Spending and Enrollment Trends Amid COVID-19. Washington, DC: Kaiser Family Foundation (KFF). Available at https://www.kff.org/coronavirus-covid-19/issue-brief/early-look-at-medicaid-spending-and-enrollment-trends-amid-covid-19/
xv Wagner J., and Solomon J. (May 27, 2020). Medicaid Coverage Protections in Families First Act: What They Require and How to Implement Them. Washington, DC: Center on Budget and Policy Priorities (CBPP). Available at https://www.cbpp.org/sites/default/files/atoms/files/5-27-20health.pdf |